Bruce’s Account of His Hospitalization
On September 9th, a Saturday, I headed out for a mid-day jog. A little four-mile loop. An old habit. A mile or so in I started to feel light-headed. I’d been feeling this way on runs for several months–years, actually, although it would go away for long periods. This year it had become more frequent and severe. I slowed to a walk to wait for it to lift, which it usually did.
The next thing I recall a police officer was accosting me: “Hey! I need you to sit down!” I remember thinking “what’s your problem?” and “fine, fine, … ” as I sat on a curb. “What’s your name?” he asked, and I thought “That’s weird, I don’t know my name.” He kept asking questions and things started to come back. An ambulance came and took me to the ER.
It turns out I had had a small heart-attack–a ventricular fibrillation, they think–passed out, fell and hit my head. A passer-by had waved down the officer who was politely but forcibly getting my attention. I’ve had an undiagnosed heart condition for twenty years. It’s resulted in several heart attacks, but I’d never lost consciousness.
The next part is a bit of a jumble. I don’t remember when I noticed my tongue hurting, but I had bit it badly. In the ER they decided to stitch it closed. They debated how many stitches to put in. Four. That hurt. Then a hematoma formed and my tongue swelled up like a balloon. They decided to intubate me before my tongue shut off my breathing. I’m sure I didn’t appreciate the significance of the intubation at the time.
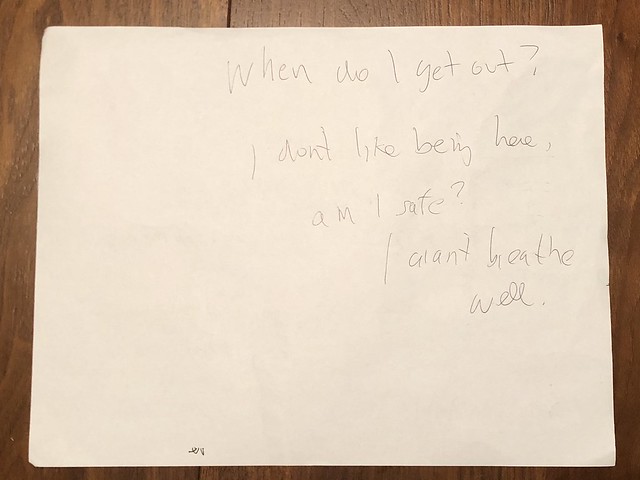
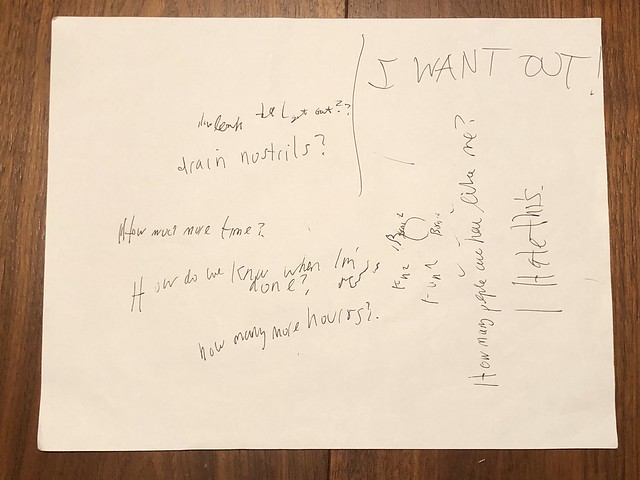
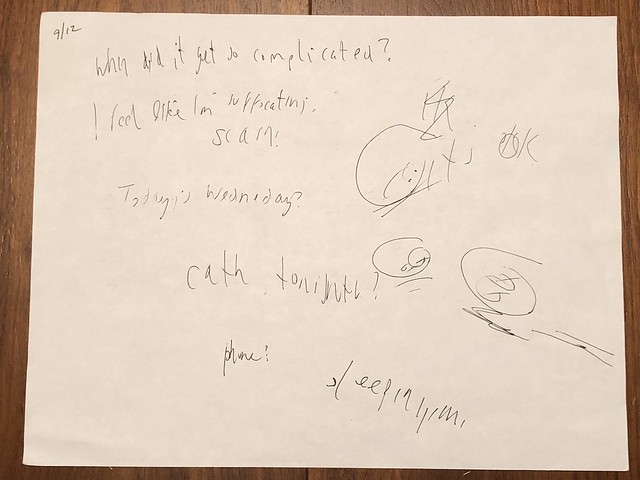
Being intubated and partially sedated was awful. I would wake and it felt like I was suffocating. Christy and the nurse kept assuring me I was safe. They’d tell me they could read my blood oxygen level and it was fine. But it felt like I couldn’t breathe, which was frightening. I’d eventually talk myself into being ok, but I’d come in and out of consciousness and every time I rewoke I’d go through it again. I really, really, wanted to get out. Throughout this time I communicated by writing on a clipboard. I’d write, to Christy, “How much longer?” and “How many more hours?” I don’t remember how she answered but she knew it was days. At some point they tied my hands down so I wouldn’t tear out the tubes but I don’t remember it.
I’ve since read that intubation can be a terrifying experience for some people. Months after I was released I had a bad sore throat and congestion, and I kept waking dreaming I was suffocating. I knew, rationally, that I could breathe, but my constricted throat brought back memories from the hospital. I had to fight panicking. Until now, I hadn’t really understood people who choose not to recall bad experiences. I’d like this memory to fade.
I slowly started to recover. A few days later they decided to extubate me. Extubation was 30 seconds of awful. They had stitched the tube to my nose to keep it from falling out and in one sequence of motions they cut those stitches and pulled the tube out. Starting to breathe again felt like choking. But progress felt great. I’d have been glad to go through much more than that. Taking the feeding tube out was easy. The urinary catheter less so. Anything in the name of progress.
I moved from the cardiac ICU to the cardiac CU, which is adjacent to the ICU. I started to walk slowly around the unit. On every loop we’d pass my cardiac ICU room. It was brightly lit, but my memory of it was as a darkened room. I even asked Christy if it was always so bright. “Yes, always.”
Christy was with me pretty much the entire time, which was unquantifiably comforting. I had a few other visitors as well, but Christy’s presence takes no effort on my part. I declined requests for most visits. I was feeling pretty dejected and not up for the pressure to be positive.
The attending cardiologist recommended a pacemaker. Actually, although I’d call it a pacemaker, it’s an implantable cardioverter defibrillator, or ICD. It does more than just re-pace you: it’s a little defibrillator with leads dangling into the chambers of your heart, watching and waiting to shock you. My regular cardiologist had brought up this possibility a few years back and at the time it was startling. I didn’t imagine I’d ever be as ill as someone who needed a pacemaker. Now they were pretty matter of fact about it. You need one. You can’t pass out. It’s dangerous. (I know I keep imagining that the worst part was passing out, and not having a heart attack, but I’m indulging some level of denial.)
I got in the queue for an ICD (I’d still yet to leave the hospital). I had to wait a few days. My roommate, a big, boisterous, overweight guy in his 60s went in ahead of me. He had traveled some way to have the procedure here, which seemed a good sign. “No big deal!” he proclaimed. I finally rolled in to have mine installed. “Hey! Welcome back!” said the nurse. I’d been there a few days earlier for a cardiac catheterization, but didn’t remember any of it. They told me I’d been funny, which I was glad to hear. It was like hearing your stand-in had represented you well.
A day or so later I finally left the hospital. Twelve days. It seemed longer. I’m still adjusting to both the severity of the event and what, if any, changes I need to make going forward. A week after being released I had an appointment with my cardiologist. They were tweaking my medication. “What about drinking alcohol? Is that ok?” I asked. “Oh, I think you could use a drink.” I’ve taken his advice.